When it comes to surgical intervention of the spine, patients are often intimidated by theprospect. We get it. It is a bit overwhelming to consider that someone (as qualified as they mightbe) will be making an incision over your spinal cord. However, advancements in spinal surgicalintervention have made so many of the procedures minimally invasive. Our board-certified spinesurgeons can improve (or even eliminate) the worst of your low back and neck pain with aprocedure at The Orthopaedic Surgery Center that allows you to go home the same day.
One of the most common procedures in the realm of spinal surgery is the microdiscectomy. Ifyou are savvy with linguistics, you may be able to guess what this procedure is intended toaccomplish. It is a small (micro) incision through which a herniated or protruding disc (disc) isremoved (ectomy). The clinical indication for such a surgery includes persistent sciatica despiteconservative management or worsening leg strength.
Patients who are candidates for this procedure have a herniated disc, whether it be from chronicrepetitive motion or one traumatic inciting event. After a work-up that includes x-rays, physicalexamination, and an MRI, a patient will likely be recommended with conservative treatmentunless weakness or pain are severe and affect one’s ability to ambulate or control their bladderand/or bowels. When it comes to the spine, we do not typically push for surgical interventionwithout at least attempting less invasive treatment. Even with recent advancements in spinalprocedures, every surgery has significant risk associated with it. If patients continue to strugglewith pain, numbness, tingling, and weakness that radiates into one or both of their legs afterformal physical therapy partnered with a short course of steroids, usually in the form of anepidural injection and relative rest, then surgical intervention is discussed.
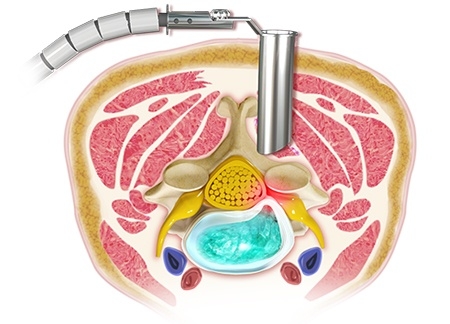
A microdiscectomy opens up a small area to allow access to the spine in the low back regionwhere the problematic disc resides. The protruded portion of the disc is then cut away so it is nolonger pushing on the nerve, which is what causes the radiating symptoms of pain, numbness,tingling, and weakness.
Most often, patients feel relief of any radiating leg pain immediately upon waking up from thegeneral anesthetic and getting out of bed. If some part of the nerve was damaged, it could takelonger to heal and see resolution of symptoms. Some incisional site pain and post-operativesoreness is common, but generally patients are feeling much improved quickly. Restrictions inthe realm of lifting and bending are present for about 2 months.
If you have been conservatively managing symptoms associated with a herniated disc with noluck, call us at Orthopaedic Associates of Wisconsin today for a consultation at our SpineCenter with one of our specialists.
This blog is written by one of our very own-Morgan. She is a certified athletictrainer working as a medical assistant with our providers each and every day inour clinic. She obtained a bachelor's degree in athletic training from CarrollUniversity in Waukesha and a master's degree in Kinesiology from MichiganState University. She is excited to bring you updates and information about thehappenings at OAW.